The Interplay of Climate Change and Vaccine Efficacy: A Public Health Crisis
Climate change is drastically impacting the distribution and effectiveness of vaccines, essential tools for public health. Extreme weather conditions threaten vaccine logistics and efficacy, while misinformation regarding vaccinations contributes to rising vaccine hesitancy. The combined effects of these issues pose significant risks, particularly in low-income countries where climate-related diseases are increasingly prevalent.
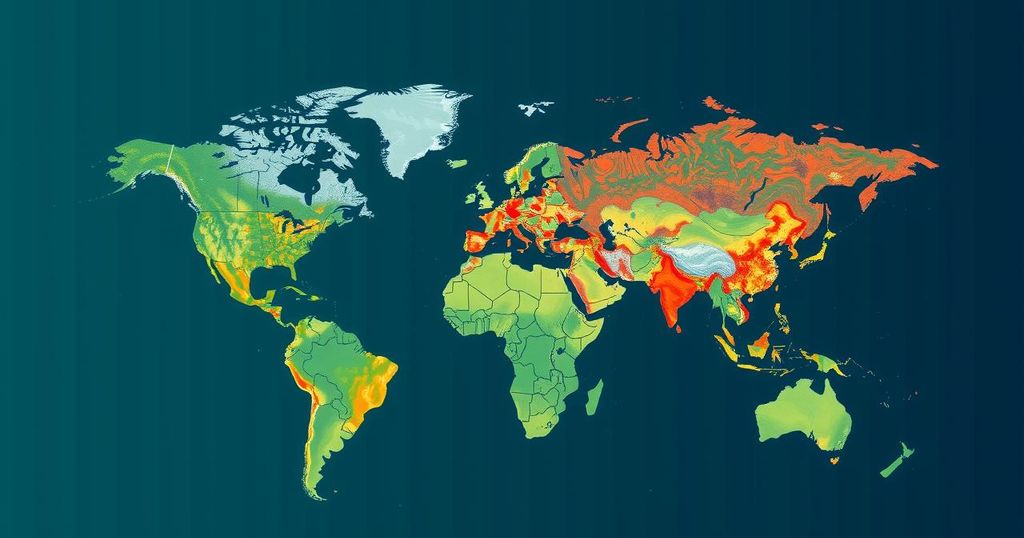
Climate change has fundamentally transformed the landscape of infectious diseases, posing significant challenges to global vaccination efforts. As extreme weather events become more frequent due to climate change, the storage and distribution of vaccines are jeopardized, reducing their overall effectiveness. The WHO acknowledges that while vaccination campaigns have saved millions of lives, they are increasingly hindered by climate-related disruptions. Concurrently, a rise in vaccine hesitancy, exacerbated by misinformation and political discourse, threatens public health just when vaccinations are most needed to combat climate-induced diseases.
The shifting climate conditions create favorable environments for bacteria and vectors responsible for diseases. Cholera outbreaks have surged worldwide, particularly in Africa, following heavy floods and adverse weather patterns. Such developments illustrate how climate change is intricately linked to disease proliferation. Research further indicates that over half of human pathogenic diseases may worsen due to climate change, thus necessitating increased immunization initiatives. However, in light of climate-related challenges, vaccination confidence is declining as misinformation spreads and skepticism towards vaccines intensifies in various communities.
The interplay of climate change and vaccine efficacy is particularly concerning. Temperature fluctuations can degrade vaccine potency, especially for vaccines that require stringent storage conditions. Moreover, adverse environmental conditions can impair immune responses, reducing the effectiveness of immunizations during peak environmental stress, such as heat waves. As vaccine misinformation proliferates, especially via social media, public confidence wanes, leading to hesitancy that complicates vaccination efforts further.
Political figures play a pivotal role in shaping public perceptions of vaccines. Individuals like Robert F. Kennedy Jr., who endorse skepticism towards vaccines, can significantly influence public health responses. His possible appointment as head of the Department of Health and Human Services adds urgency to address vaccine hesitancy and misinformation. The consequences of vaccine skepticism in conjunction with climate change could result in increased disease prevalence and correspondingly diminished public health outcomes. Governments must demonstrate transparency and address these challenges with integrity and commitment to science.
The context of this article centers on the intersection of climate change and public health, specifically how global warming influences disease patterns and vaccine distribution. The World Health Organization estimates the significant impact of vaccines in protecting public health over the decades. However, with climate change contributing to extreme weather events, the vulnerability of vaccine supplies is heightened. Concurrently, growing vaccine hesitancy fueled by misinformation poses a formidable barrier to achieving adequate immunization coverage, particularly in low-income regions that are disproportionately affected by climate-related health threats.
In summary, the challenges presented by climate change significantly hinder public health initiatives, particularly vaccination efforts. Climate-induced disruptions threaten vaccine efficacy, while rising vaccine hesitancy fueled by misinformation further complicates immunization strategies. Addressing this dual crisis necessitates an urgent response from public health officials and policymakers, emphasizing the importance of factual information and trust in vaccination programs. Ensuring that communities are well-informed and protected against the impacts of climate-fueled diseases relies heavily on transparent governance and proactive health policies.
Original Source: www.nationalobserver.com






